Recurrent pregnancy loss / Recurrent miscarriages

Miscarriages are very common. More than half of miscarriages are related to chromosomal abnormalities in the fetus, and are sporadic (do not tend to recur). However, some couples suffer from recurrent miscarriages. This can be a frustrating situation and warrants medical evaluation to find out any cause and help to guide treatment.
Definition: Recurrent pregnancy loss / Recurrent miscarriage is defined as a condition in which there are two or more pregnancy losses.
Prevalence: It affects 1-2% of couples worldwide. Most of the miscarriages happen during the first trimester (within the first 13 weeks of pregnancy), and only a few are during the second trimester (within 14 to 24 weeks of pregnancy).
Causes and risk factors
In half of the cases there is an identifiable cause, which may be:
- Parental chromosomal abnormalities (balanced translocation): 2%-5%
- Uterine abnormalities (including congenital uterine anomalies, adenomyosis and cervical incompetence): 10-15%
- Autoimmune disorders and thrombophilia (including antiphospholipid syndrome): 15-20%
- Endocrine diseases, e.g. diabetes mellitus, polycystic ovary syndrome, and thyroid disorders: 15%
- Idiopathic: 50% (Maternal obesity may be one of the risk factors.)
Other risk factors for miscarriages include parental age, obesity, smoking and drug abuse.
Suggested investigations to consider:
- Couple: karyotype (blood test)
- Wife:
- Autoimmune markers (test for antiphospholipid syndrome)
- Thyroid function test and thyroid autoantibodies
- 3D USG of pelvis to look for abnormalities in the uterus and evidence of polycystic ovaries
- Karyotyping of products of gestation (if available)
- Blood glucose if risk factor is present
- Husband:
- Sperm DNA fragmentation test
Half of the couples with a history of recurrent miscarriage do not have an identifiable cause, despite investigations. In this situation, the chance of a successful future pregnancy ranges from 50 to 80%, with maternal age being one important factor.
Management options
Causes:
- Parental chromosomal balanced translocation:
- Occurs in less than 5% of couples with recurrent miscarriage.
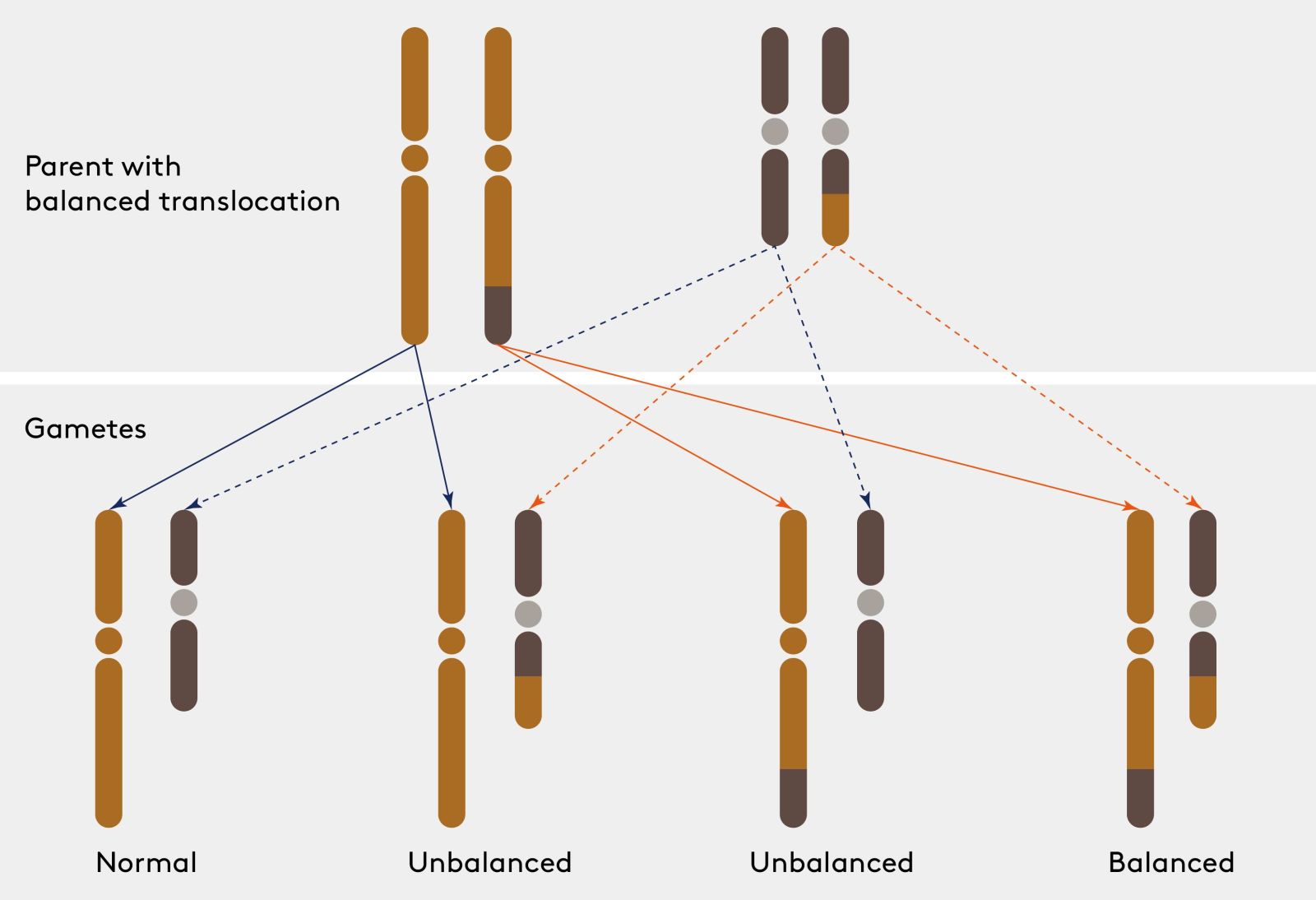
- One of the partners may carry a chromosomal defect called a ‘balanced translocation’ (no loss or gain of genetic material).
- The fetus is at risk of ‘unbalanced’ translocation (with genetic loss or gain), which will very likely end up in miscarriage.
- ‘Sporadic’ chromosomal abnormalities: The couple has normal karyotype, but fetal chromosomal abnormalities may still occur, especially with advanced age.
- Advanced maternal age is associated with an increased risk of meiotic non-disjunction and hence aneuploidies. It increases the risk of recurrent miscarriage.
- Advanced paternal age is also associated with a higher chance of DNA fragmentation of sperms and therefore abnormal embryos that are more easily miscarried.
Investigation:
Karyotyping of the parents, which will reveal the balanced translocation; Sperm DNA fragmentation test
Treatment:
Fertility treatment with pre-implantation genetic testing or donor gametes may be considered.
Uterine abnormalities
Congenital uterine abnormalities include septate uterus, bicornuate uterus and unicornuate uterus. It may impair implantation and hinder embryo growth, leading to infertility or miscarriage.
Investigations:
- 3D transvaginal ultrasound scan
- Hysterosalpingogram or hysteroscopy
- Magnetic resonance imaging (MRI)
Treatment:
- Surgery to correct the problems in the uterus may be considered, e.g. division of uterine septum.
Autoimmune diseases
A few autoimmune diseases, e.g. antiphospholipid syndrome (APS), are associated with recurrent miscarriage.
In APS, the immune system produces abnormal antibodies that attack phospholipids in blood and increases the risk of thromboembolism. This interferes with blood flow to the placenta, and may stop the pregnancy from continuing properly in the uterus, leading to miscarriage.
Investigation:
- Antiphospholipid antibodies including lupus anticoagulant (LA)
- Anticardiolipin antibody (ACA IgG and IgM)
- Anti-β2-glycoprotein I antibodies
Treatment:
- A woman who fulfil the laboratory criteria of APS (two positive results of antiphospholipid antibodies in blood taken at least three months apart) and with a history of three or more consecutive pregnancy losses may be prescribed low-dose aspirin (75 to 100 mg/day) before conception, and a prophylactic dose of heparin starting on the day of her first positive pregnancy test.
Thrombophilia
Hereditary thrombophilia is a very rare condition in which the risk of venous thromboembolism is high and therefore the risk of miscarriage is higher.
Treatment: Low-dose aspirin (75 to 100 mg/day) before conception, and a prophylactic dose of heparin should be prescribed starting on the day of her first positive pregnancy test.
Cervical incompetence
Less than 1% women have a weakness in the cervix that allows it to dilate too early. Typically, cervical dilatation from cervical incompetence is not associated with uterine contractions. Rupture of membranes and intra-uterine infection may occur as a result of cervical incompetence. It usually causes second trimester miscarriage or preterm delivery.
There may be a previous history of cervical surgery (e.g. LEEP or cone biopsy for CIN).
The diagnosis is based on history.
Cervical length measurement showing a short cervix is suggestive but not diagnostic of cervical incompetence.
Treatment: Typical cervical incompetence should be managed with cervical cerclage, which is usually performed during the early second trimester (16- 20 weeks) or late first trimester (12-13weeks). Some selected cases may be offered cerclage before conception.
Preimplantation Genetic Testing (PGT)
 1100 x 680.jpg)
PGT is carried out when the embryos are at the blastocyst stage (day 5) after IVF+ICSI treatment, where a few cells will be biopsied for genetic testing. While the biopsied cells are being analysed, the embryos are frozen, and will be transferred to the uterus once they are confirmed to be normal.
PGT-A
A procedure used prior to implantation to help screen abnormality in chromosome number (known as aneuploidy) within embryos created through in vitro fertilization to reduce the chance of miscarriages due to aneuploidies.
Indications:
- Advanced maternal age (35 years old or above)
- Recurrent pregnancy losses
- Repeated embryo transfers without pregnancy
- Severe male infertility
PGT-SR/M
A procedure used prior to implantation to help identify chromosomal structural rearrangements (PGT-SR) and single gene defects (PGT-M) within embryos created through in-vitro fertilization to prevent certain diseases or disorders from being passed on to the child.
Indications:
- Either or both partners are carriers of single gene mutations that may affect health of a future child.
- Either partner has a chromosome rearrangement (called a translocation) that can result in genetically abnormal eggs or sperm.